How surprised would you be to discover that Europe’s largest employer is described as “riddled with racism” (Nagesh 2022)?
Racism is integrated into everything us humans create, from A.I. to healthcare services. This is evident in historical and current reports of global majority NHS staff experiences (Somra, Warmington MBE, & Kline, 2024), racial disparities in service user health outcomes (National Perinatal Epidemiology Unit 2023, Race Equality Foundation 2019), racial disparities in access to culturally tailored healthcare (cite), and racially motivated pseudoscience (Saini 2019; Harvard 2022; Evans 2018; Ben-Cheikh et al. 2021). Individuals and organisations have a moral, social, and legal responsibility to recognise this and take proactive and consciously inclusive steps to eliminate racism in healthcare.
Racism harms employee health and well-being, career opportunities, staff and service user retention, and innovation rates. This article centres on qualitative and quantitative data-led insights highlighting the reality of racism in UK healthcare and some long-term and short-term consequences on individuals and healthcare services. It concludes that there are numerous opportunities for development and culture change.

Global Majority Staff Experiences
The report, Too Hot To Handle: An Investigation Into Racism In The NHS, produced by Roger Kline, Joy Warmington MBE, and Ghiyas Somra, explores experiences of non-white staff raising concerns around reports of racism (2024). Of the 1,300 global majority respondents that participated in the survey, 75.7% shared they avoided raising a racial discrimination concern due to the belief that nothing would change. Of the respondents who shared they had raised a concern following racial discrimination, only 5.4% said that their concern was taken seriously and managed in a satisfactory way.
Lack of Culturally Inclusive Approaches to the Provision of Care
Where healthcare professionals are not expected to, or supported to, develop a racially equitable education of health and wellbeing, it is unlikely that they will find themselves equipped with the knowledge or skills to do so. A recent publication by Massie et al. (2021) revealed a stark disparity in the representation of non-white individuals in medical literature. From 1992 to 2017, only 18% of images featured in the New England Journal of Medicine included non-white skin tones. This lack of representation disproportionately erases the diverse experiences of global majority communities and reinforces the implicit bias prevalent in medical education and practice.
Mental Health Act Statistics, Annual Figures – 2020-21 highlights alarming statistics regarding the disproportionate detention rates among Black, Asian, and Minority Ethnic (BAME) communities under the Mental Health Act (NHS 2021). Rates of detention for Black or Black British groups are over four times those of White groups, while Community Treatment Orders for the same demographic are over ten times higher than for White groups. These disparities underscore systemic racial bias within mental health services, where individuals from BAME backgrounds are more likely to be subject to coercive measures (NHS 2021).
Another concerning finding from the same annual figures captures the overrepresentation of Black people in restrictive interventions within hospital settings (2021). Black people are more than four times more likely to be the subject of “restrictive interventions” (2021), such as being restrained or held in isolation while in hospital. Thus, racially inclusive approaches must prioritise de-escalation techniques, trauma-informed care, and alternative interventions that provide equitable care and treatment.

Racial Disparities in Service User Health Outcomes
Not only does medical racism impact staff members, but it also has a direct impact on patient outcomes and standards of culturally informed care. The alarming statistic that the UK maternal mortality for Black birth givers is nearly four times higher than for White birth givers, as reported by the National Perinatal Epidemiology Unit in Maternal Mortality 2019 – 2012, underscores the urgent need for targeted interventions (2023).
Mental Health and Wellbeing in England Adult Psychiatric Morbidity Survey 2014 found racial disparities in mental health outcomes are also evident. The 2019 study Racial Disparities in Mental Health: Literature and Evidence Review revealed that Asian or Asian British-Pakistani men exhibit the lowest recovery rates for IAPT talking therapies(2019). These findings emphasise the reality of UK healthcare provisions that widely exclude the needs of the global majority.
Consequences
The consequences of racism in the NHS include capital losses, negative impact on staff mental health and wellbeing, rising attrition rates, reduced clinical confidence, and diminishing service user confidence.
Recent studies by Roger Kline and Professor Duncan Lewis reveal a staggering financial loss of £2.3 billion annually in the NHS due to bullying and harassment. Dr Chaand Nagpaul, the former Chair of the British Medical Association, has emphasised that racism is a significant driver behind these figures (2023). This financial toll can influence the operational efficiency of the NHS.
The British Medical Association’s Racism in Healthcare Report underscores the devastating toll racism takes on the mental health and well-being of healthcare professionals. 60% of doctors who reported experiencing racism detailed profound negative impacts on their mental health, including depression, anxiety, increased stress levels, lowered confidence and self-esteem, as well as various physical health issues (2022). Such profound effects can not only hinder individual performance but also erode the overall resilience of the workforce.
The Racism in Healthcare Report reveals that 23% of respondents admitted to considering leaving their jobs due to racial discrimination, with an additional 9% leaving as a result (2022). This high turnover rate disrupts the continuity of care service users receive and undermines healthcare teams’ stability and cohesion. Addressing racism is crucial for retaining talent and fostering a supportive working environment.
Research conducted by Harris and published in the National Library of Medicine highlights a trend of reduced confidence among healthcare practitioners when treating patients from global majority backgrounds. Specifically, healthcare participants reported feeling less confident in assessing, managing, and diagnosing skin conditions in darker skin tones (2023). This lack of confidence can jeopardise the quality of care provided and perpetuate disparities in health outcomes. It is imperative to raise awareness of this development need and invest in cultural competency training and resources to mitigate these disparities and ensure equitable healthcare delivery for all patients.
Public Health England’s findings indicate a theme of diminished confidence among BAME service users, accompanied by reports of fear when accessing healthcare services (2020). This fear stems from experiences of racial discrimination and mistreatment, leading to reluctance to seek timely medical attention. This barrier to healthcare can exacerbate existing health inequalities. There is a clear need to urgently pursue culture change within UK healthcare settings aiming to rebuild trust and ensure equitable access to healthcare. (Public Health England 2020, 23; Keeting et al. 2002)

Solutions
It is imperative for healthcare professionals and NHS HR staff to proactively engage in initiatives that address and rectify racial disparities, ensuring equitable health outcomes for all service users.
How can RightTrack Learning help?
RightTrack Learning provide a range of learning and development opportunities led by experienced diversity and inclusion training consultants. These range from off the shelf solutions, designed to cater to healthcare providers, to bespoke training tailored and designed in collaboration to your specific needs.
Our off-the-shelf Racism in Healthcare Training for clinical and on-clinical medical professionals is designed to raise awareness of how racism practically manifests in healthcare, equipping you with a solid foundation to create informed proactive change. The learning objectives for this course include to:
- Understand the terminology relating to race, ethnicity, and culture.
- Recognise what is meant by scientific racism, medical racism, racial discrimination, and personal bias.
- Appreciate the reality of racism and privilege in healthcare for both service users and staff members.
- Explore the impact of racism within healthcare on medical practice, society, and service users.
- Know our responsibilities in challenging the status quo.
- Have a set of actions to encourage anti-racism beyond the session.
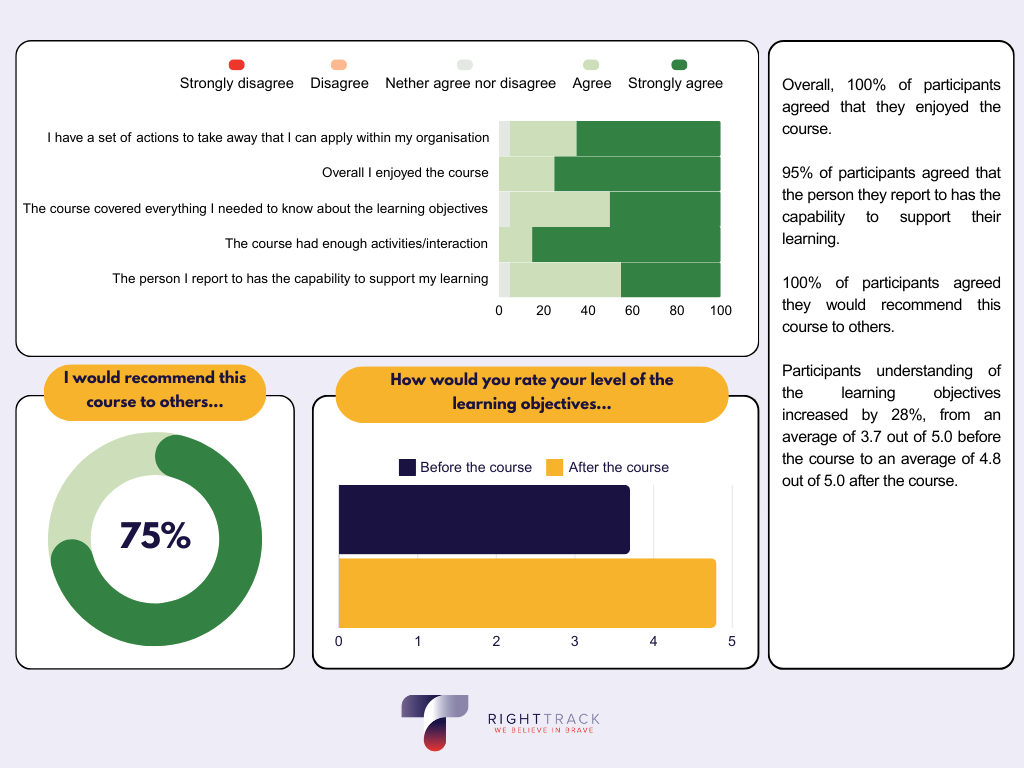
The feedback we’ve received from past medical professionals attending this course has been overwhelmingly positive. See below for a high-level look – highlighting the impact our training sessions have on attendees understanding of the learning objectives, experience of the course, and the impact this learning has on intentional plans for behavioural change.
When asked ‘what will you do differently as a result of attending the course?’ the participants answered:
- Action my plans to keep up-to-date with racism.
- As per action plan, actively consider including others with different protected characteristics when forming groups/teams; follow a more diverse group on social media.
- Be conscious of my own bias and some fast thinking decisions.
- Be more aware of my unconscious bias and be more conscious inclusive.
- Be more aware of my unconscious biases.
- Be more reflective and try to understand my bias.
- Change the way I think and act at work to be more inclusive.
- Feel more comfortable with micro affirmations.
- Further reading re: the implicit association test.
- I need to do more reading and thinking about practical ways to apply. More of example of how to do this would be great.
- I will be careful to check my own micro aggressions and how my automatic thinking can lead to these being expressed and received by my colleagues, patients and students.
Bibliography
(2020). Beyond the data: Understanding the impact of COVID-19 on BAME groups. In Public Health England (Ed.), www.gov.uk/phe (pp. 1–69). PHE publications. https://assets.publishing.service.gov.uk/media/5ee761fce90e070435f5a9dd/COVID_stakeholder_engagement_synthesis_beyond_the_data.pdf.
Ben-Cheikh, I., Beneduce, R., Guzder, J., Jadhav, S., Kassam, A., Lashley, M., Mansouri, M., Moro, M. R., & Tran, D. Q. (2021). Historical Scientific Racism and Psychiatric Publications: A Necessary International Anti-racist Code of Ethics. Canadian journal of psychiatry. Revue canadienne de psychiatrie, 66(10), 863–872. https://doi.org/10.1177/07067437211020613.
Bignall, T., Jeraj, S., Helsby, E., and Butt, J (2019) Racial disparities in mental health: Literature and evidence review. https://raceequalityfoundation.org.uk/wp-content/uploads/2022/10/mental-health-report-v5-2.pdf.
British Medical Association. (2022). Racism in medicine [Review of Racism in medicine]. In bma.org.uk (pp. 1–43). British Medical Association. https://www.bma.org.uk/media/5746/bma-racism-in-medicine-survey-report-15-june-2022.pdf.
Evans, G. (2018, March 2). The unwelcome revival of “race science.” The Guardian; The Guardian. https://www.theguardian.com/news/2018/mar/02/the-unwelcome-revival-of-race-science.
Exclusive: Racism is costing NHS billions – EasternEye. (2023, July 5). https://www.easterneye.biz/exclusive-racism-costing-nhs-billions/.
Harrison J. (2023). A scoping review exploring the confidence of healthcare professionals in assessing all skin tones. British paramedic journal, 8(2), 18–28. https://doi.org/10.29045/14784726.2023.9.8.2.18.
Harvard University. (2022). Scientific Racism. Harvard Library. https://library.harvard.edu/confronting-anti-black-racism/scientific-racism.
Keating, Frank & Robertson, David & McCulloch, Andrew & Francis, Errol. (2002). Breaking the circles of fear.
Kline, R., Warmington, J., & Somra, G. (n.d.). Too Hot To Handle?: why concerns about racism are not heard… or acted on. In www.brap.org.uk (pp. 1–66). brap and Kline.
Massie JP, Cho DY, Kneib CJ, Sousa JD, Morrison SD, Friedrich JB. A picture of modern medicine: race and visual representation in medical literature. J Natl Med Assoc. 2021;113:88-94.
Nagesh, A. (2022, February 2). NHS “riddled with racism” against ethnic minority doctors. BBC News. https://www.bbc.co.uk/news/uk-60208523.
NHS. (2021, October 26). Mental Health Act Statistics, Annual Figures – 2020-21. NHS Digital. https://digital.nhs.uk/data-and-information/publications/statistical/mental-health-act-statistics-annual-figures/2020-21-annual-figures.
Public Health England (2020) Beyond the data: Understanding the impact of COVID-19 on BAME groups.
Saini, A. (2019). Superior: The Return of Race Science. Beacon Press.
University of Oxford. (2023, October). Maternal mortality 2019-2021: MBRRACE-UK: NPEU. The National Perinatal Epidemiology Unit. https://www.npeu.ox.ac.uk/mbrrace-uk/data-brief/maternal-mortality-2019-2021#:~:text=The%20risk%20of%20maternal%20death,%2D20%20(Figure%203).